WHO should lead on genome-editing policy, advisers say
A committee formed in the wake of a scandal has advised the World Health Organization (WHO) to assume a leading, global role in efforts to regulate genome editing. The WHO should help governments to coordinate their country-level regulations, the advisers say, and genome editing should not yet be used to make modifications that can be passed on to later generations.
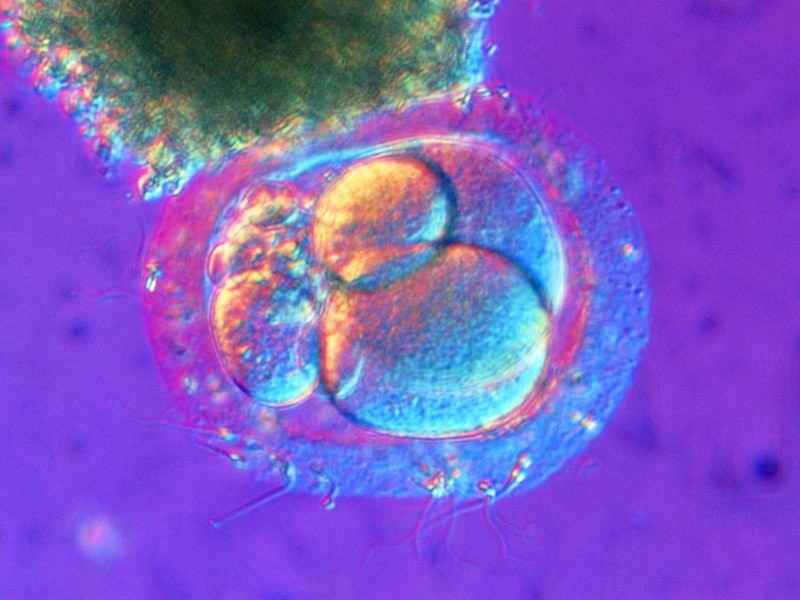
The recommendations, released in two separate reports on 12 July, are the culmination of two years of work by the advisory group. It was formed after biophysicist He Jiankui, formerly at the Southern University of Science and Technology in Shenzhen, China, shocked the world in 2018 by announcing that he had used the CRISPR genome-editing technique to alter embryos that were implanted and led to the birth of two girls.
The committee’s mandate was to tackle the thorny issues raised by unchecked genome editing — but without quashing its medical promise. Among its recommendations are to foster international collaboration in the governance of such applications, to encourage appropriate ethical review of clinical trials involving human genome editing and to promote equitable access to medicines that are developed using the technology.
The recommendations are not legally binding, but they still have the power to shape deliberations among governments and funding bodies around the world, says Julian Hitchcock, a lawyer at London firm Bristows, who specializes in the regulation of regenerative and reproductive medicine. “They set a standard,” he says. “At that level, I think that they are quite significant.”
After He’s 2018 announcement, a host of researchers and scientific organizations called for a moratorium on the use of genome editing to create heritable changes to the human genome. In 2019, WHO advisers recommended the creation of a registry of clinical studies of genome editing in humans, and said it was too soon to proceed with clinical applications of germline genome editing, as He had done. The WHO does not have the power to impose moratoriums on specific research practices, but a number of countries and funding agencies already have moratoriums on germline genetic editing in place.
And in September 2020, another committee — convened by the US National Academy of Medicine, the US National Academy of Sciences and the UK Royal Society, and with representatives from ten countries — also concluded that the technology is not yet ready for use in human embryos destined for implantation.
The new reports from WHO advisers reiterate their 2019 position against heritable editing at this time, and urge international collaboration in the governance of other applications of the technique. Clinical trials of genome editing have shown promise in treating blood disorders such as sickle cell anaemia, cancer and a deadly genetic disorder called transthyretin amyloidosis.
Such applications are not conceptually far from other approaches to gene therapy, such as inserting entire genes into the genome, says Hitchcock. And several countries, including the United Kingdom and United States, already have robust regulations around gene-therapy trials and medicines, he notes.
But there are concerns that these applications of genome editing could be too expensive for use in many countries where they’d be most beneficial: sickle-cell anaemia, for example, is particularly prevalent in sub-Saharan Africa. The WHO advisers called for consideration of how intellectual-property rights will affect pricing of genome-editing therapies — an important first step in discussions about equitable access, says Kay Davies, a geneticist at the University of Oxford, UK .
WHO advisers also recommended that the United Nations create a working group to evaluate the implications of emerging technologies, including genome editing. Such a committee would be a key endorsement for international collaboration, says Davies. “You can’t dictate to different countries what they should do — there are going to be big cultural differences between them,” she says. “But if we learn from each other, it’s going to be important.”
By sidestepping specifics, however, the committee missed an opportunity for greater clarity around key issues, says bioethicist Abha Saxena at the University of Geneva in Switzerland. It was a missed opportunity to make concrete suggestions on governance structure and on issues that affect lower-to-middle-income countries, she says.
And the reports urge the WHO to regularly evaluate such technologies as they progress. “I hope that will be reflected in national laws,” says Hitchcock. “There’s a problem if you produce regulations and the science catches up — the regulations get out of date, fast.”
https://www.nature.com/articles/d41586-021-01922-y