Top 10 COVID-19 Infographics of 2020

Every week, we identify the top search term or phrase, based on increased interest from medical professionals. We then compile the findings that most likely made that topic popular and present them, along with an infographic based on the most relevant clinical information.
Unlike in years past, one single subject dominated almost all of 2020: COVID-19. Looking back at the most popular clinical topics related to the pandemic is not only a reminder of major events from the recent past but an indicator of what information is still needed and what concerns are most significant among doctors, nurses, and students moving ahead.
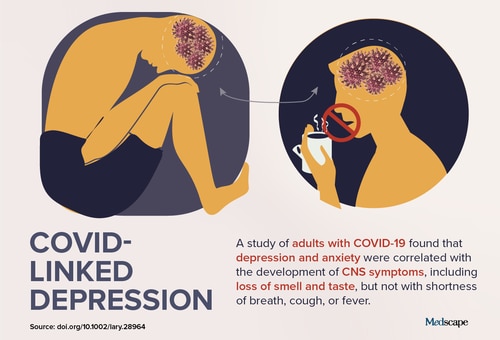
10. COVID-Linked Depression
In mid-August, healthcare professionals were focused on a "staggering" increase in COVID-linked depression and anxiety. Data from a voluntary online mental health screen, released by Mental Health America (MHA), found a dramatic increase in depression, anxiety, psychosis, and suicidality. As of the end of June, more than 169,000 additional participants had reported having moderate to severe depression or anxiety, compared with participants who completed the screen before the pandemic. In June alone, 18,000 additional participants were found to be at risk for psychosis.
In a press release, Paul Gionfriddo, president and CEO of MHA, said, "The problem is bigger than anyone imagined." The biggest problems were seen among adults younger than 25 years. Approximately 90% screened positive for moderate to severe depression, and 80% screened positive for moderate to severe anxiety.
A separate, cross-sectional study of more than 100 adults with COVID-19 found that depression and anxiety may reflect penetration of the central nervous system by the novel coronavirus. The findings suggest that changes in mood could indicate more than an emotional response to the disease itself. The researchers concluded that depression and anxiety "may be harbingers of more dire COVID-19 outcomes."
Long-term effects of these mood changes and mental health issues are particularly concerning, as one third of outpatients with COVID-19 are unwell weeks later. According to survey results from the Centers for Disease Control and Prevention, 35% of adults with symptomatic coronavirus infection had not returned to their usual state of wellness when they were interviewed 2-3 weeks after testing. Psychiatric conditions, such as depression, were significantly correlated with prolonged recovery.
Experts discussed an "echo pandemic" of mental illness and suicide that may be coming in the wake of COVID-19. Lorenzo Norris, MD, assistant professor of psychiatry and behavioral sciences at George Washington University, described the combination of economic, social, and health threats occurring simultaneously as the equivalent of "getting hit by an earthquake, a tsunami, and a famine at the same time."
As the pandemic has continued, concerns about lingering mental health effects have only increased. A focus on mood changes in particular made COVID-linked depression the tenth overall top trending clinical topic of 2020.
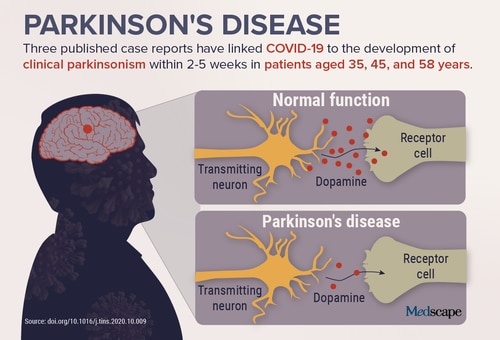
9. Parkinson's Disease
A reported link to COVID-19 and new options for diagnosis and treatment helped make Parkinson's disease a top trending clinical topic in late November. An article published in Trends in Neurosciences examined the mechanisms potentially at play in three relatively young patients with COVID-19 who developed clinical parkinsonism. For two of the three, parkinsonism symptoms diminished after administration of traditional dopaminergic medication. The third patient recovered spontaneously. In all cases, brain imaging showed reduced function of the nigrostriatal dopamine system, as is seen in Parkinson's disease. None had a family history of the condition, and one patient underwent genetic testing and was found not to carry any of the risk variants.
The authors of the article believe that COVID-19 may predispose patients to develop Parkinson's disease either sooner or later. Although these cases do not prove a causal relationship between the two conditions, the researchers say the potential of long-term neurologic sequelae supports the idea that COVID-19 should be treated as aggressively as possible.
In terms of preventing Parkinson's disease, a study suggested that coffee consumption is associated with a reduced risk in a particular subset of individuals. The study showed that caffeine levels were lower in patients with Parkinson's disease compared with controls, but this difference was much greater in individuals with a mutation in the leucine-rich repeat kinase 2 (LRRK2) gene. The authors suggest that if the findings are confirmed in additional studies, caffeine-related therapies may help reduce the development of the condition in individuals with the LRRK2mutation.
In more encouraging news, Parkinson's disease may soon be diagnosed using a skin test. Researchers used a chemical assay to detect clumping of the protein alpha-synuclein, which is a hallmark of the condition, in autopsy skin samples. Those samples were taken from patients whose condition had been confirmed by brain pathology. The skin testing showed a high degree of sensitivity and specificity for the diagnosis of Parkinson's disease. If the results are replicated in live patients, the skin test could facilitate quicker diagnosis and the ability to start preventive treatments that slow disease progression before severe symptoms develop.
A development in treatment also received attention in November. A study found that apomorphine sublingual film was efficacious and generally safe and well tolerated for the on-demand treatment of off episodes in Parkinson's disease. Although the sublingual film had more oral adverse effects than the injectable form, it may offer some advantages in terms of administration during off episodes. For example, the new formulation is more convenient than carrying an injection, as it comes in a small, tear-open packet that contains a medication strip the patient places under their tongue.
From COVID-related concerns to new developments in prevention, diagnosis, and treatment, various findings contributed to Parkinson's disease becoming the ninth overall top trending clinical topic of 2020.
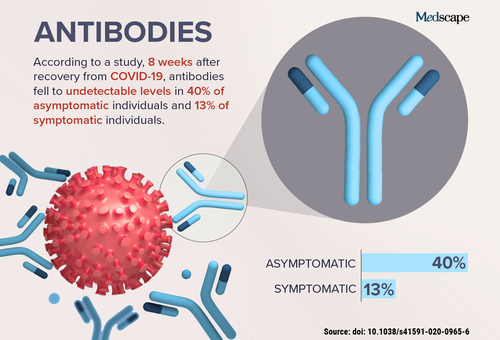
8. Antibodies
In early July, issues surrounding the antibodies developed after COVID-19 infection became the top trending clinical topic. A study from China found that people who develop antibodies after becoming infected with SARS-CoV-2 may not retain them for more than a few months. This was especially true for individuals with asymptomatic infection.
A separate study of patients from New York found that although the majority of those studied did produce antibodies after coronavirus infection, 33% of individuals tested had antibody titers that implied having no immunity to repeat infection. Since those studies were published over the summer, other reports have presented similar findings.
Antibody testing may also play a role in assessing whether COVID-19 has invaded the brain. A small case series of three patients in a US hospital who had COVID-19 and encephalitis found that although only one had abnormal white blood cell or protein levels in the cerebrospinal fluid, all had evidence of IgM antibodies. Lead author Karima Benameur, MD, says the findings suggest that CSF test results that indicate normal levels of inflammatory proteins do not necessarily mean that the virus has not entered the brain. She recommends CSF IgM testing, if possible, to confirm brain involvement in these patients.
As interest shifts towards vaccine response and whether individuals who have had COVID-19 still require vaccination, antibodies are likely to remain an incredibly important focus, just as they were over the summer.
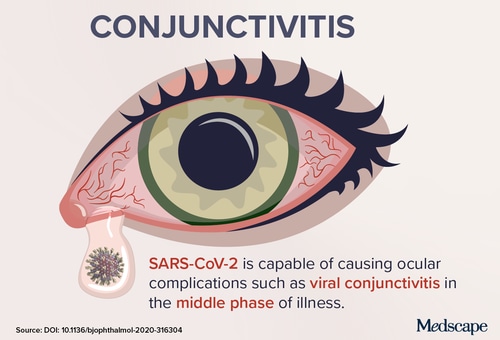
7. Conjunctivitis
Although all medical specialties have been affected in some way by COVID-19, ophthalmologic concerns were the focus in early June, when conjunctivitis related to infection with SARS-CoV-2 was the most popular topic. H. Nida Sen, MD, director of the Uveitis Clinic at the National Eye Institute in Bethesda, Maryland, suggested then that people with conjunctivitis should be tested for coronavirus infection. Several studies also found evidence that the virus may cause "pink eye."
A report in the British Journal of Ophthalmology described a 30-year-old man with confirmed COVID-19 and bilateral acute conjunctivitis. Conjunctival swab specimens remained positive for SARS-CoV-2 on days 14 and 17 after symptom onset. The authors stressed, however, that conjunctival sampling may not be useful for early diagnosis of COVID-19 because the virus may not initially appear in the conjunctiva.
Contracting COVID-19 through the eye was a subject of much scrutiny. A survey found that ophthalmology was one of the top three specialties associated with a greater risk of medical residents contracting SARS-CoV-2. Notably, Li Wenliang, MD, who risked his job to spread warnings about COVID-19, was an ophthalmologist and died after contracting the virus from an asymptomatic patient.
Because of reports of conjunctivitis in patients with COVID-19 and concerns about disease spread through the eye, the American Academy of Ophthalmology (AAO) issued updated guidance. The information stresses that, because patients with conjunctivitis frequently present to eye clinics or emergency departments, ophthalmologists may well be the first clinicians to examine patients with COVID-19. As such, the AAO emphasized proper safety precautions, including the use of disposable tonometer tips, because SARS-CoV-2 was found in the tears of patients with conjunctivitis.
Ophthalmologic concerns related to the ongoing pandemic helped make this specific condition the seventh overall top trending clinical topic of 2020.
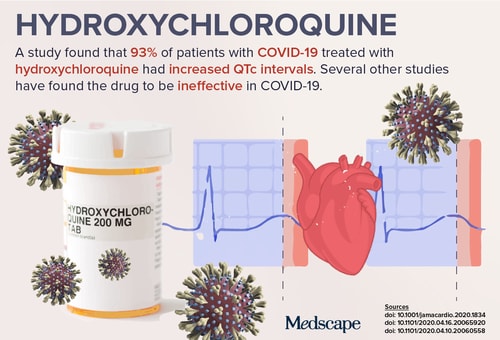
6. Hydroxychloroquine
Perhaps no drug received more attention and controversy this year than hydroxychloroquine. In May, as clinicians scrambled to identify any agent that may be useful in treating COVID-19, concerns about the antimalarial drug made it a top trending clinical topic.
Many of the clinical trials conducted earlier in the year did not include ECG assessment to either exclude people at high risk of developing a cardiac arrhythmia or to identify patients who develop a dangerous QTc interval during use of hydroxychloroquine. Two studies released on May 1 provided evidence of the risk for serious arrhythmias.
A study from Boston of 90 patients with confirmed COVID-19 treated with hydroxychloroquine found that 23% had notable prolongation of QTc intervals. One of the patients developed torsades de pointes after treatment with a combination of hydroxychloroquine and azithromycin. The second study, which was from France, found that 37 of the 40 patients (93%) with COVID-19 treated with hydroxychloroquine had some increase in QTc interval, but none of the patients developed an identified ventricular arrhythmia.
Elsewhere, a study of 150 hospitalized adults in China found that hydroxychloroquine does not help clear the SARS-CoV-2 virus or relieve the symptoms of COVID-19. The findings of the Chinese researchers were echoed by results of a retrospective study of Veterans Affairs patients hospitalized with COVID-19, which showed that hydroxychloroquine with or without azithromycin did not reduce the risk of requiring mechanical ventilation. It also found an increased risk for death associated with the administration of hydroxychloroquine alone.
In late April, the US Food and Drug Administration (FDA) released a communication stating that "the FDA is aware of reports of serious heart rhythm problems in patients with COVID-19 treated with hydroxychloroquine or chloroquine, often in combination with azithromycin and other QT-prolonging medicines. We are also aware of increased use of these medicines through outpatient prescriptions." The agency reiterated that treatment with hydroxychloroquine and chloroquine in patients with COVID-19 should occur only in a hospital and when participation in a clinical trial is "not available" or "not feasible."
The quest to identify useful and safe treatments for COVID-19 is ongoing. Hydroxychloroquine is the sixth overall top trending clinical topic of 2020, but any useful medication is likely to surge in popularity in 2021.
Read more about drugs and therapies used in treating COVID-19.
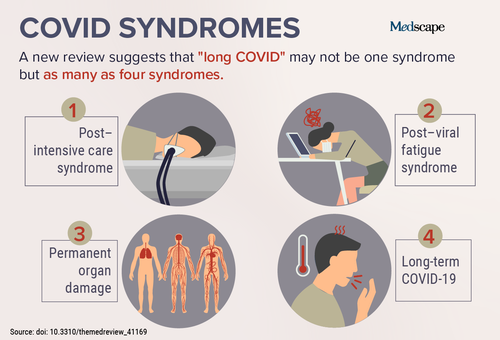
5. COVID Syndromes
Findings and related developments associated with the condition known as "long COVID" resulted in a top trending clinical topic in October. A review of available scientific evidence on individuals with prolonged COVID-19 symptoms, published by the National Institute for Health Research, found that long COVID may not be one syndrome but as many as four. The paper included analysis of recurring symptoms among hospitalized and nonhospitalized patients with COVID-19. Ongoing problems were reported with the respiratory system, brain, cardiovascular system and heart, kidneys, gut, liver, and even skin.
Although many patients recover within 2-3 weeks, a growing number of long COVID cases have been reported. Experts have expressed concern about whether enough is being done to study and treat long-term effects of COVID-19. Investigators are exploring possible relationships between long COVID, myalgic encephalomyelitis/chronic fatigue syndrome, and other viral illnesses.
Even for those who are not considered long-haulers, recovery from COVID-19 can be difficult. Exercise tolerance may take 2-3 months or longer to return to baseline. Heart-related symptoms, such as residual palpitations and persistent tachycardia, have been reported without any residual inflammation in the blood. The scope of the potential problem is also significant. As one expert pointed out, given the millions of cases, if even 10% have long-lasting symptoms, that would mean hundreds of thousands of new patients who require ongoing care would enter health systems around the world.
Beyond the long-term physical effects, the lasting psychological impact of COVID-19 was given the name "coronaphobia." Although the term is a catchall for the anxieties and concerns experienced in reaction to the pandemic, researchers have formalized a definition of the long-term mental health effects. Some literature suggests that coronaphobia is more likely among those who feel vulnerable to disease, are predisposed to anxiety, or struggle with uncertainty.
Although many who care for patients with COVID-19 remain immersed in short-term concerns, long-term issues are increasingly a subject of interest. This explains why "COVID syndromes" is the fifth overall top trending clinical topic of 2020.
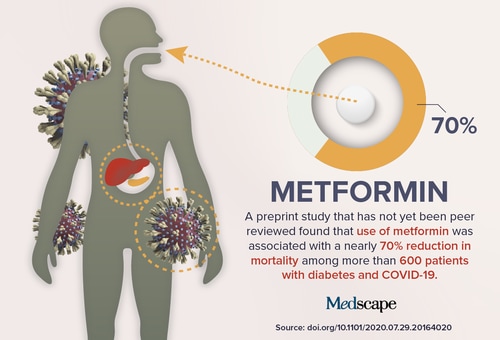
4. Metformin
In late August, curiosity about a potential role in COVID-19, along with studies exploring other benefits and adverse effects, made metformin a top trending clinical topic.
The most commonly prescribed drug for type 2 diabetes (T2D) may be associated with reduced risk for death due to COVID-19. Results of a recent study were published online and showed a significant reduction in mortality among patients with diabetes and COVID-19 who used metformin. These findings support the results of four previous studies that also showed a reduction in mortality among metformin users compared with nonusers. However, experts say that the randomized controlled trials needed to conclusively prove this benefit are "almost impossible in the context of COVID-19."
Other possible benefits of metformin outside of coronavirus-related issues have been explored. A retrospective observational study of more than 5000 patients with T2D, published this spring, found that older adults who received preoperative metformin had higher 90-day survival rates and fewer readmissions than those who were not taking the drug. A separate, small retrospective study found that metformin may also help improve motor function in individuals with diabetes and Parkinson's disease. Also earlier this year, an observational study from South Korea found that metformin was associated with a reduced risk for death and end-stage renal disease among people with T2D who have chronic kidney disease.
The news wasn't all positive, however. Research out of the United Kingdom found that metformin use was associated with increased rates of moderate anemia in patients with T2D. This finding was consistent across two randomized controlled trials and replicated in one real-world study of routinely collected data. In one of the studies, each 1 g/d of metformin use was associated with a 2% increased annual risk for anemia.
Questions about its potential role in COVID-19 and studies investigating both benefits and potential adverse effects made metformin the fourth overall top trending clinical topic of 2020.
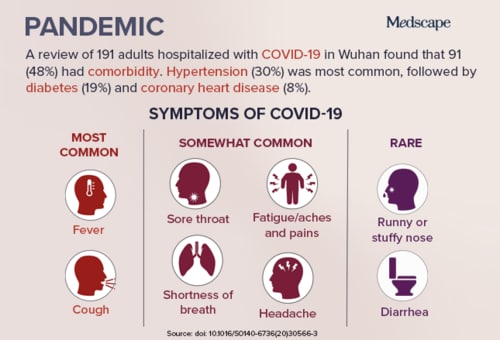
3. Pandemic
On March 11, the World Health Organization formally declared the COVID-19 outbreak a pandemic, which expectedly resulted in that term becoming the most popular clinical topic. Although new symptoms have been added to the list, this infographic from early spring shows those symptoms first reported to be associated with COVID-19, along with initial findings regarding comorbidities and disease severity.
Early on, one of the major concerns was the high mortality rate seen in certain individuals. A study published in the Lancet examined adult inpatients with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital who had been discharged or died by January 31. The review found that patients who did not survive hospitalization were more likely to be older and to have comorbidities and elevated D-dimer levels. Showing signs of sepsis on admission, comorbidities such as hypertension and diabetes, abnormal blood clotting, and the prolonged use of noninvasive ventilation were also important factors that contributed to increased mortality.
An editorial published in late March in The New England Journal of Medicine suggested that the mortality rate associated with COVID-19 may actually be "considerably less than 1%," as opposed to the 2% reported by some groups. The editorial was published alongside a report of laboratory-confirmed COVID-19 cases, which found a mortality rate of 1.4% among 1099 patients. However, authors of the editorial suggested that the number of asymptomatic or minimally symptomatic cases is probably several times higher than the number of reported cases, which would lower the fatality rate significantly below 1%.
COVID-19 and related subjects are most likely to stay among the top trending clinical topics well into next year. You can find the latest COVID-19 news and guidance in Medscape's Coronavirus Resource Center.

2. COVID Toes
Unusual dermatologic symptoms associated with COVID-19 resulted in a top trending clinical topic in early May. The American Academy of Dermatology is one of many societies that launched registries to share information about COVID-19 cases. "COVID toes" were among the more commonly reported dermatologic manifestations. Lesions that appear on the feet of patients with COVID-19 have been described as resembling those seen in individuals exposed to cold temperatures. Many of the reported cases initially involved children.
Around the same time in spring, atypical symptoms were also reported among older adults with COVID-19. Characteristic symptoms of fever, cough, and shortness of breath were noted to be absent in some elderly patients, who instead simply seemed "off" soon after becoming infected with the coronavirus, sleeping more often than usual, acting apathetic or confused, and being disoriented to place. Neurologic symptoms were also described in May among other populations, with encephalopathy, ataxia, and even strokes first associated with COVID-19. In New York City, one neurosurgery department reported five cases of large vessel stroke over a 2-week period among patients with COVID-19 who were younger than 50 years. That is a sevenfold increase over what normally is seen.
Around that time, anosmia became an increasing concern. Results of a study published in the International Forum of Allergy & Rhinology showed that 68% of patients with COVID-19 had olfactory impairment and 71% had taste impairment, whereas only 16% and 17% in the control group experienced loss of smell or taste, respectively.
Many months later, the connection between COVID-19 and various symptoms is still being explored. Although the presence of "COVID toes" has yet to be added to official guidance, the dermatologic finding received a great deal of attention, becoming this year's second overall top trending clinical topic.
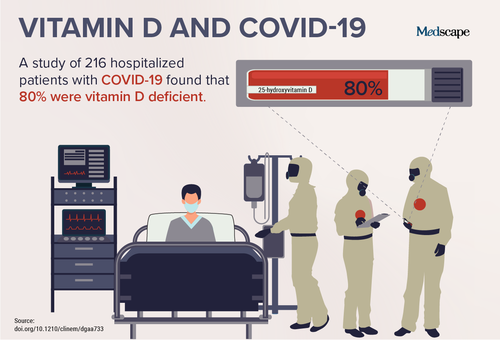
1. Vitamin D and COVID-19
As researchers continue to explore its possible association with COVID-19, vitamin D emerged as a top trending clinical topic in early November. A study published in the Journal of Clinical Endocrinology & Metabolism found that serum 25-hydroxyvitamin D [25(OH)D] levels were lower in hospitalized COVID-19 patients than in population-based controls.
These findings came after separate research found that patients hospitalized with COVID-19 who had sufficient vitamin D levels had significant reductions in severe outcomes and a lower risk for death compared with those who had insufficient levels. Yet another study found that individuals in the United States with sufficient vitamin D levels had as much as a 54% reduced risk of becoming infected with COVID-19.
Still, the exact nature of the relationship between vitamin D levels and COVID-19 remains unclear. Experts point to similar complicated findings seen with other diseases. Low levels of vitamin D have been reported in a wide variety of conditions, from multiple sclerosis to cancer, with little evidence that supplementation does much to prevent disease or control severity. However, a small randomized trial found that vitamin D may have helped reduce intensive care unit (ICU) admission among hospitalized patients with COVID-19 from 50% to 2%.
Whether vitamin D is beneficial in ICU outcomes in general remains uncertain. Last year, a trial found no statistical benefit when a 540,000 IU boost of vitamin D was administered to 2624 critically ill patients. Regardless, the potential benefit during the pandemic has prompted investigations of supplementation in key populations, such as residents of elder care homes. A study published in BMJ Nutrition, Prevention & Health found glaring gaps between recommendations for vitamin D supplementation and actual practice in this population. Because that group is at particular risk for severe outcomes associated with COVID-19, experts are calling for increased efforts to achieve adequate vitamin D levels.
Researchers caution that vitamin D has not been established as clearly protective against contracting COVID-19 or preventing a severe disease course. However, the possibility that a readily available supplement with few known significant adverse effects may be beneficial captured wide attention, resulting in 2020's top trending clinical topic.